I’m writing to inform you of an ordeal Jan and I have been experiencing for the past few months that you might benefit from in knowing the outcome. In the latter part of 2020, we received notice from Blue Cross and Blue Shield of North Carolina that our individual qualified high deductible health care plan will increase in premium to about $1870 per month. Do the math; that is $22,440 per year for a high deductible health plan to be associated with an HSA. My annual deductible under this plan is $7000 and Jan’s annual deductible is $7000. So, our total annual liability would be $22,440 plus $14,000.
We could “save money” by going to a Blue Cross and Blue Shield of North Carolina group plan. We considered this in past years, but Blue Cross’s rules are such that our agency would need to be an S corporation. As it stands our agency has been a proprietor, LLC. To switch to an S corporation would mean a total restructure of our business, learning QuickBooks, and many of the complexities which avail nothing other than “saving money” on our group health insurance. By the way our premium would drop from around $1870 to $1200 for us both for the same coverage, same network, and same liability, $7000 deductible for each. So, we bought QuickBooks and we applied for Blue Cross group coverage, effective 1-1-2021.
We do not take a lot of medicines, but I take a solution medication called Clobetasol. It is for itchy scalp. I’m allowed one bottle each month. I had been paying about $44 per month per bottle and I had been buying it from a local independent pharmacy in Harrisburg called Harrisburg Hometown Pharmacy. The entire $44 was going towards our high deductible, and I was happy. We switched plans effective January 1, 2021 but for my January prescription for the solution, it filled for the old $44 price, still in the system.
Earlier this week I asked Jan to stop by the pharmacy and pick up my February prescription. She did, and she informed me that the price was $123! Nothing changed except we went from a Blue Cross and Blue Shield of North Carolina individual policy to a Blue Cross and Blue Shield group policy, so we thought. I immediately called the pharmacy and Blue Cross to check with them to see if there was a problem. The only problem was that my formulary under the group plan was nowhere near as good as the formulary under the individual plan. Remember, we have no copays; this is discounting.
[In Blue Cross’s Defense, North Carolina laws do permit carriers to write a 1-person group [yes; a 1-person group is an oxymoron], but most group carrier do not, due to their lack of profitability. Apparently, Blue Cross is offsetting its losses on this plan by using its unusually austere formulary.] This is not to say that ALL BCBSNC group formularies are this way.
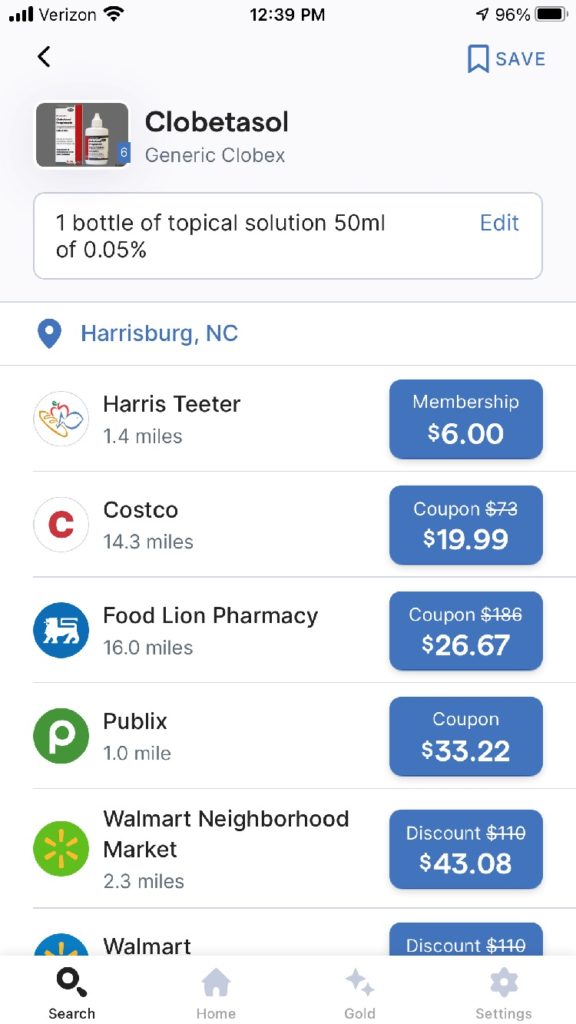
While I was speaking to the pharmacist, I pulled out my iPhone and went to the GoodRX app to look up Clobetasol and you can see the below image as to what I saw. Through my local Harris Teeter, who has apparently joined a program with Kroger, I could fill my Clobetasol prescription for $6 per month in their club. Club membership is $36 per year per individual and $72 to be able to add 6 more ‘anybodies.’ That breaks down for one to approximately $3 per month fee on top of $6 per month co-pay, essentially. They happily gave me this pricing over the phone, not even knowing who I was.
As a last-ditch effort to try to remain with Blue Cross and have my purchase of my prescription drug funnel through and under my exorbitantly high annual deductible. I reached out to my Blue Cross online service which is called Alliance to see what their pricing would be if I ran the script through them. They told me that they cannot give me pricing until the prescription had switched or transferred to them. I asked them, “what sense does that make?” Why go to the trouble to transfer something if I don’t know the price? But, I took them at their word, and last Friday actually initiated the transfer. But I was told by them Friday to call Monday, which is today, to get the pricing. I needed to do this because whether I would be happy with their pricing or not the script would go through if I did not call to intervene in the process. I asked how could this be as the script has already been filled for February. I got no real answer. Juxtapose this lack of transparency from MY CARRIER to the good folks at Harris Teeter.
So, I called today to the online people at Blue Cross Alliance, and really got nowhere. I was told that since the script itself would not transfer until March, they would not be able to release pricing until then. This is the point that I gave up on my insurance company.
I called the people at the 800 number inside the Kroger discount club website. [The HT link sends you to the Kroger site. They are compatible.] They are extremely helpful. They signed me up for their annual membership for $36 and immediately sent me to confirmation emails with all my individual information in the club, a group number, and prescription bin number. They told me my price would be $6 each month for the prescription, but it gets better!
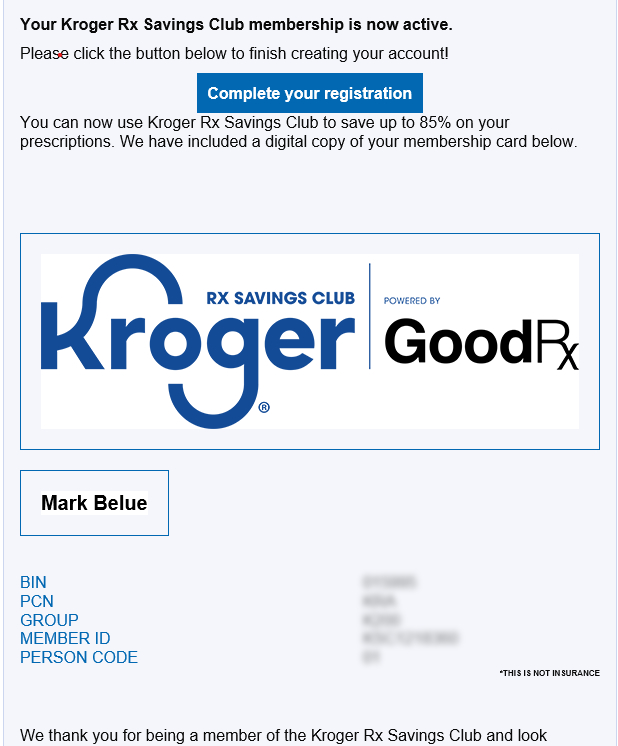
They said that I could put in a request for the Clobetasol to be filled every 90 days and they would drop one of the $6 copays [Not really copays, but that is what I am calling them]. In the end, had I remained with Blue Cross and paid $123 per month, my total annual cost would be $1476 for 12 of those little white bottles. However, through Harris Teeter my cost will be $36 + (12 X4) = $84. Madness! And, at this price, I bet they are still making money.
I thought I would pass this information on to you. Thank you.
P.S.: Maybe Jan will let me go buy something? Mirrorless Canon camera?
